Cardiologist Visit with 300+ Cholesterol on Low-carb Diet
My journey avoiding commonly prescribed statins with a high LDL on a low-carb diet. The decision process supported by my cardiologist, CAC, CIMT, NMR tests.
Since I said enough with yoyo diets and chose low-carb diet as a lifestyle my (total and LDL) cholesterol levels skyrocketed. As of today, I lost 40+ pounds while increasing my muscle strength significantly. I feel great but my test results warranted a cardiologist visit as cholesterol is complex enough for primary physicians to provide a reasonable guidance. Being on a low-carb diet makes it an even more complicated matter for the traditional medical system.
The earliest cardiologist visit was available a couple months later. So this allowed me to go there prepared and know what is expected from the visit in advance: starting statin as a treatment. As my life is on the line (in either accepting or rejecting statin), I had to do the research, collect the data and present them to the doctor and decide the next steps without any bias. As an engineer, I approach health as an engineering problem. So I was hoping to meet a doctor that would play along with this workflow.
Here are the things I have done prior to the cardiologist appointment:
CAC: Calcium Score Test
This CT scan test reveals the calcification which is called the hard plaque in the arteries. It reveals the damage already done by your lifestyle so far. My result was 0, yes, zero calcification in my arteries. It was quite a relief. But my understanding is that this test looks at the past rather than present. Soft plaque is another even more dangerous risk factor causing heart attacks. So I was looking for another test to detect this soft plaque: CTA (Coronary CT Angiogram) [1] or perhaps CIMT (carotid intima-media thickness test).
NMR test
The lipid test primary physicians request in annual visits is deemed antiquated by most researchers as it does not tell the whole store. NMR blood test deep dives into LDL and provides great insights into LDL particles and their size. It also gives an insulin resistance score. My NMR test revealed a super high number of LDL particles as I expected. But the size of the particles were in the healthy range which is great news. I was also proud of my insulin sensitivity (very low insulin resistance score) which is the result of my intermittent fasting and low carb diet.
Historical Cholesterol Values vs Body Weight
This is something I did as a flash of genius in the clinic waiting room. I have marked my elevated LDL levels with red and normal LDL levels with green on my body weight chart that spans multiple years.
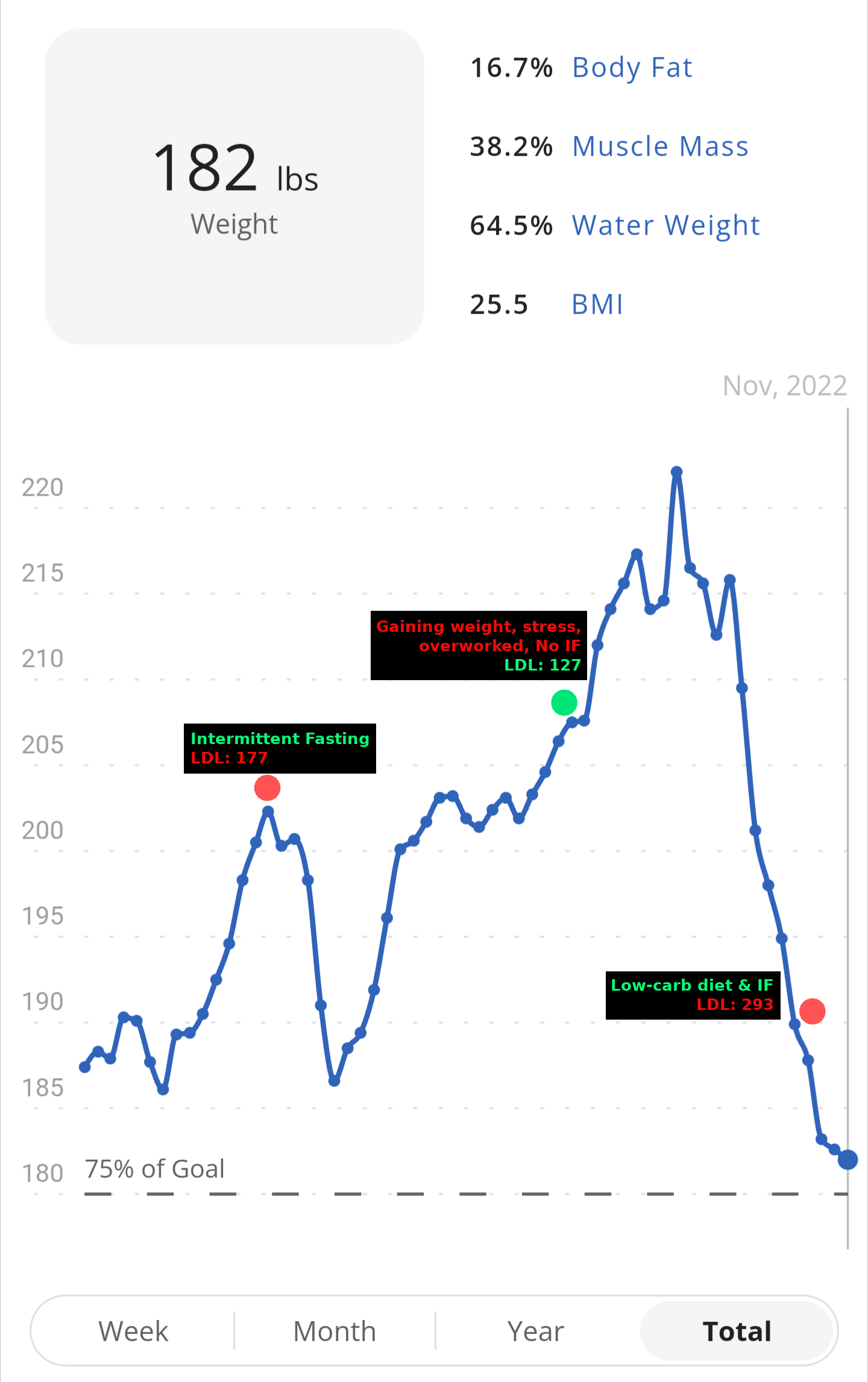
The result was very interesting. When I started intermittent fasting (not even low-carb diet) in 2019 my LDL was elevated to a level my primary physician recommended statins for the first time. After two years in 2021, when I was rising in the ranks from overweight to obese after I gave a break to intermittent fasting eating carbs, desserts coupled with lack of sleep, over-working and lack of exercise, my primary physician was congratulating me on bringing my LDL to a healthy level through “healthy diet”. And finally in 2022 I doubled down on good habits once again and incorporated my later longevity tips into my own lifestyle; and wait for it; my LDL skyrocketed! So my LDL was inversely correlated with my BMI and well-being.
After some research, here is my theory which I also shared with my cardiologist. LDL is like a cargo ship carrying triglycerides (energy in the form of fat), cholesterol (repair material for tissues) and vitamins. When I am doing intermittent fasting and/or a low carb diet, fat becomes my primary source of energy. So the liver is loading the LDL with triglycerides. As I hit the gym hard and break my muscles, there is a greater need for cholesterol to reach those broken muscle tissues and fix them. The liver ends up creating more LDL to keep up with this increased demand. These are the symptoms of a well functioning body which itself is an engineering marvel.
The Plan to Lower Cholesterol
I devised two contingency plans:
Bad Plan: I could devour some high carb foods such as pizza, burger, french fries prior to next test (which would spike my insulin that locks down fat burning mechanism) and stop weight-lifting (which reduces the demand for cholesterol in the muscle tissues). This is a bad plan because it would take a week for me to get back to a healthy lower glycogen level. But I am confident that this will work as I am not the first engineer to notice this fact (see Dave Feldman).
Good Plan: After reaching my ideal body weight and fat percentage (below 15%) in a couple of months, I won’t have much visceral fat to burn (the very reason why very low body fat percentages require more commitment). This will naturally reduce the LDL particle number. Going into maintenance mode at the gym will also reduce the cholesterol demand causing the liver to wind down on LDL production.
The how part of the good plan includes some measures such as replacing 6 whole eggs with 1 whole egg + 5 egg whites in my breakfast. This measure is not because dietary cholesterol causes elevated LDL; there are well established researches showing that this is not true (see Peter Attia). It is because I want my body to tap more into body fat rather than dietary fat for energy to reach my goal faster. Regardless I didn’t want to challenge the doctor with latter part; relatively recent research.
The Great Day: Cardiologist Visit
I introduced myself with the high LDL problem while doing intermittent fasting, a low carb diet, walking minimum 15k steps a day and hitting the gym every week day. As a side note, I told the doctor I surpassed my past strength levels of 10-20 years ago in the military: doing 4 sets of 10 pull ups then vs now doing the same with 25lbs attached to me.
It was my lucky day! The doctor was an open minded physician. He thanked me for bringing additional test results (NMR and CAC). My LDL levels on the weight chart also helped him rule out “familial hypercholesterolemia” written on my file as I could manipulate my LDL without any medication. Zero calcium level together with larger LDL particle size and the fact that I am feeling great and strong made him confident that I will be just fine without statins. He also acknowledged that low-carb is relatively new and as physicians they are trying to learn about these special cases. We decided to follow up the result of my good plan above. The doctor ordered another NMR and CIMT (carotid intima-media thickness test) for the next visit.
My experience was great and it was unlike my wife’s visit to the cardiologist with the similar LDL values a few weeks earlier. Her cardiologist pushed for statins. When my wife asked them to order CAC and NMR tests, her cardiologist's response was the same: statins even if the CAC says zero plaque and NMR particle size comes okay. It got me by surprise that her cardiologist did not even talk about checking blood sugar and insulin resistance first to justify their recommendation.
It is obvious that medical science is established on the assumption that humans have to live on a high carb diet with 3+ meals a day. When you confront the system with the opposite, the solutions from their playbook becomes quite irrelevant if they obediently follow the guidelines. So it really comes down to knowing your vitals, parameters and establishing the correlation among those yourself before surrendering to the antiquated, rigid guidelines.
Side note for the reader: if you are not doing intermittent fasting and/or low carb-diet, and still getting high LDL you’d better listen to standard guidelines your doctor is recommending as the above conversation does not apply to you.
References:
1: https://desertmedicalimaging.com/news/closer-look-heart-using-ct-scan-coronary-artery-disease/